Gut Flora Health – The Ongoing Microbe Battle

Gut Bacteria / Wikimedia Commons / Public Domain
As we go throughout our day, a war is being waged inside of us. This war takes place between our gut flora, a number of bacterial species and fungal life forms, among others. Overall, these microscopic organisms make up what is known as the microbiome. Some of these creatures are symbiotic in nature, while others have a negative effect on our health and overall well being.
The first person to recognize the association between an imbalanced gut flora and ill health is Nobel laureate Elie Metchnikoff, who said, “toxic gut flora can speed up aging and cause disease.”
Michael Snyder, PhD, further exemplifies this statement by saying, “the microbiome is associated with every disease, diabetes, cancer, autism.”
With that said, we should focus on creating a healthy, symbiotic microbiome within us and expect good health to follow us throughout life.
We Are Our Bacteria
Bacteria Cells / Wikimedia Commons / Public Domain
According to a 2007 study, there are over 100 trillion bacterial cells within the human body.[i] It is estimated that bacteria cells outnumber human cells 10 to 1. In addition, bacterial DNA outnumbers human DNA 100 to 1.[ii] In other words, we really are our bacteria. Now that the human genome has been sequenced and analyzed, scientists are beginning to focus their attention on the multitude of bacterial strains that inhabit the human body in order to obtain a better understanding of human biology.
In order to put this in perspective, the microbiome as a whole has more weight than the liver.[iii] Since its collective weight is the size of an organ, it should be treated and studied as such.
During childbirth and nursing, bacterial colonies begin to take form throughout our body and create our microbiome. In fact, half of our current microbiome can be attributed to our mother’s microbiome and the other half to our lifestyle choices.[iv] Ultimately, these bacteria dictate who we are, what we think, and regulate our very existence.[v] Those who have an empire of healthy gut flora that can easily fight off pathogenic bacteria and fungi have the potential to remain in a disease free state throughout life.
Within our colon alone are about 3 pounds of bacteria, consisting of over 400 different species, predominated by Bifidobacterium.[vi] This jungle like ecosystem consists mainly of anaerobic bacteria that are attached to the mucosa. These bacteria maintain cleanliness in the colon by disposing of decaying and diseased cells, among other things. Those who have colonies of probiotic bacteria that line their intestinal walls don’t allow pathogenic life forms the space to colonize.
What Does The Gut Flora Do?
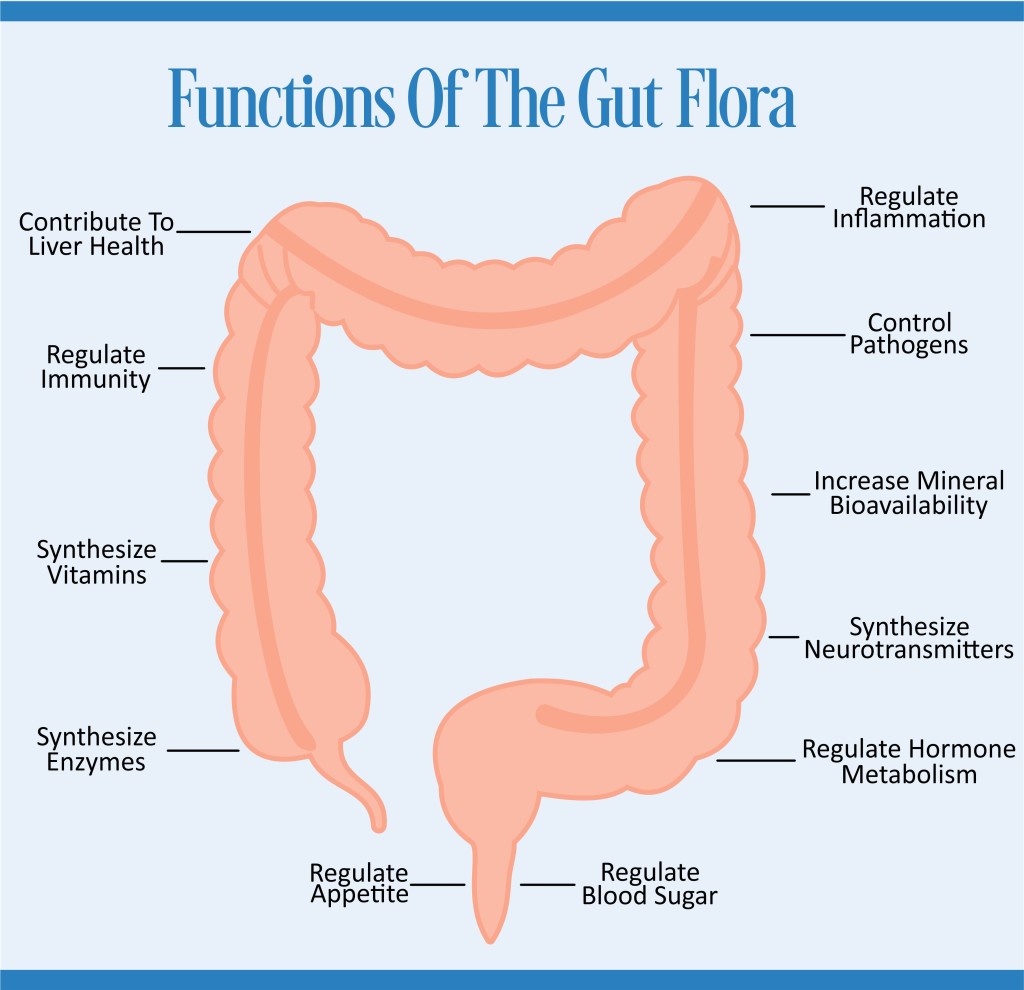
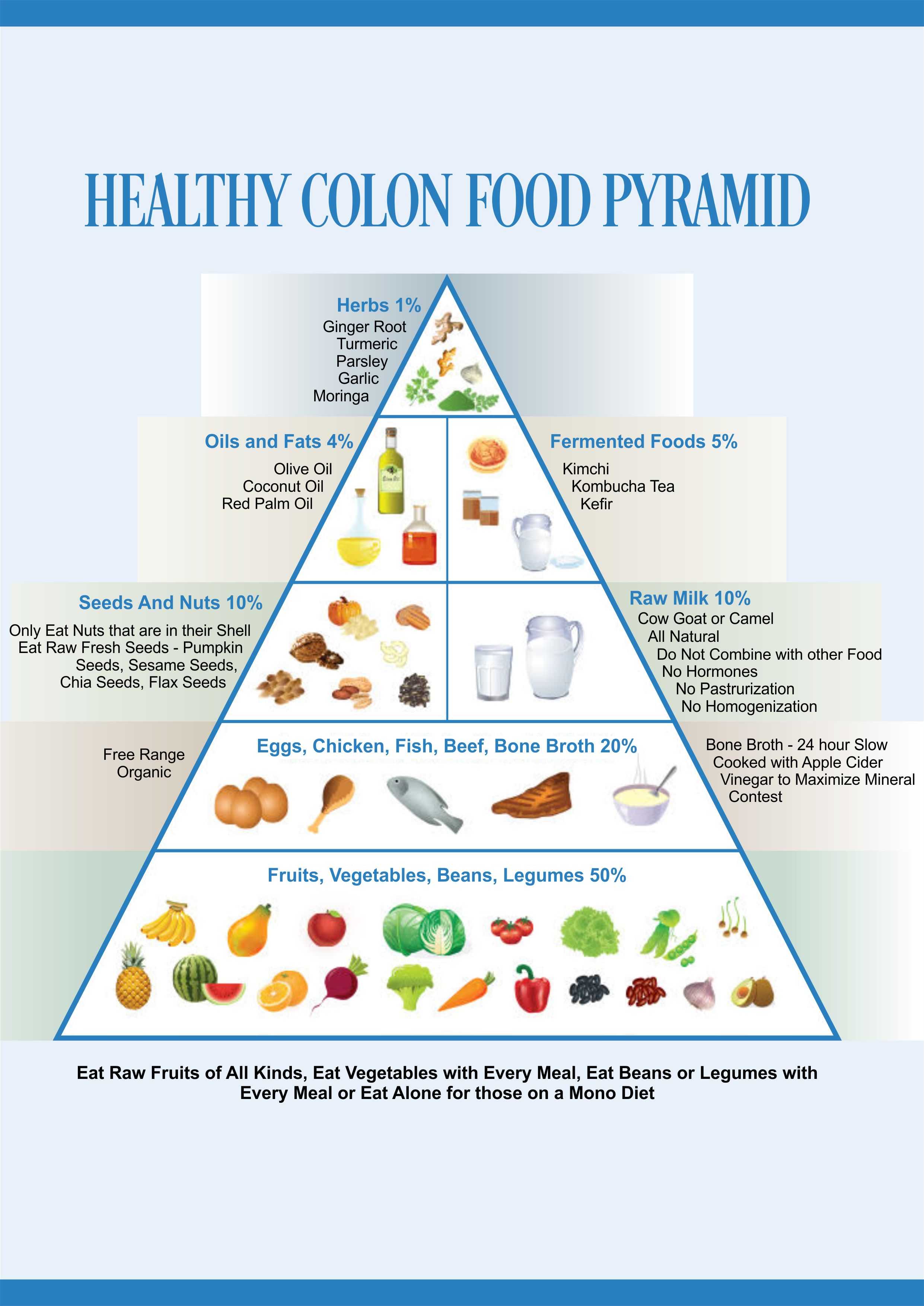
Share the Functions of the Gut Flora On Your Site
The gut flora controls pathogens, regulates immunity, regulates inflammation, synthesizes vitamins, synthesizes enzymes, increases mineral bioavailability, synthesizes neurotransmitters, regulates hormones metabolism, regulates blood sugar, regulates appetite, and contributes to liver health.[vii]
A healthy intestinal flora provides a barrier between the epithelial cells of the colon and pathogenic bacteria, known as colonization resistance.[viii] In other words, these probiotics colonize the entire colon wall effectively reducing space for pathogenic bacteria to take hold or even break through the intestinal wall.
These bacteria also synthesize certain vitamins, like B7, biotin, B12, folic acid and vitamin K.[ix] In addition, the gut flora produces enzymes that are secreted into the epithelial cells of the colon, allowing various bodily functions to take place.
The healthy bacteria within the intestines also create molecules for the brain, otherwise known as metabolites. This contributes to healthy brain function, as healthy bacteria have an effect on neurological function.[x]
The intestinal flora receives its nutrients from mucin, a glycoprotein that is excreted by the mucous membranes.[xi]
Bacteria also ferment indigestible carbohydrates, otherwise known as dietary fiber, like pectin, cellulose and hemicellulose into short chain fatty acids.[xii] These fatty acids are a great source of energy for the body and contribute to healthy epithelial cell proliferation.
Bacterial – Brain Connection
Brain and Gut / Wikimedia Commons / Public Domain
The gut has been considered the second brain, as it has more neuron cells than the spinal cord.[xiii]
The gut flora also makes neurotransmitters like serotonin and dopamine.[xiv] It can therefore communicate with the brain and controls a large number of processes within its realm.
With that said, the next time you have a “gut feeling”, go with it.
Factors That Affect Good Bacteria
Those who live a healthy lifestyle and eat natural foods generally have a sufficient number of good bacteria residing within them. Those who maintain this healthy state have the potential to avoid chronic diseases associated with pathogenic bacteria and a Candida overgrowth.

Antibiotics / Wikimedia Commons / Public Domain
There are a number of factors that can affect probiotic bacterial levels. The biggest negative effect on bacterial levels in general is antibiotic abuse.[xv] Those who have been through a number of different antibiotic regimens likely have displaced their natural bacterial balance. Other problems that contribute to bacterial dysbiosis include excessive use of laxatives and heavy metal toxicity, generally from dental amalgams or pollution. In addition, environmental pollutants, corticosteroids, chemotherapy, radiation, antibacterial soap, toothpaste, shampoo, and detergents all affect bacterial levels, among other things.[xvi]
All in all, the biggest contributor to dysbiosis is antibiotics use so we will focus on that in detail. Even those who have never consumed antibiotics may be accumulating antibiotic residue from meat and milk. Since 80% of all antibiotic use in the United States is used on farm animals, it is important to consume food that has been certified organic.[xvii]
Some other factors that contribute to unbalanced bacteria levels include long bouts of diarrhea, as it has the potential to wash out healthy colonies.
In addition, too much fiber has the potential to destroy healthy bacteria. The reason for this is because bacteria ferment fiber into short chain fatty acids, ethanol and lactic acid, among other products. A large concentration of ethanol has the potential to destroy bacteria.[xviii]
Upstream Gut Flora Disrupters
Further up the digestive system, a sluggish pancreas may not secrete the necessary pancreatic enzymes in order to neutralize acid from the stomach. This overly acidic matter has a potential to kill gut bacteria and potentially cause an ulcer.[xix]
On the other side of the coin, low stomach acid has the potential to allow colonization of bacteria in the upper small bowel. Low stomach acid also contributes to heartburn through a negative feedback loop and allows for undigested food to pass through the digestive system.[xx] Those with low stomach acid levels should change their lifestyle and if need be, supplement with betaine hydrochloric acid.
Antibiotics And Their Effect On Gut Flora
Those who don’t take part in an immediate probiotic inoculation after antibiotics have been consumed will likely have problems associated with a bacterial imbalance throughout life.
After killing off both good and bad bacteria through antibiotic use, it is a scramble to re-colonize the colon.[xxi] If pathogenic bacteria are able to take hold of this breeding ground, they are allowed to multiply and contribute to various problems.
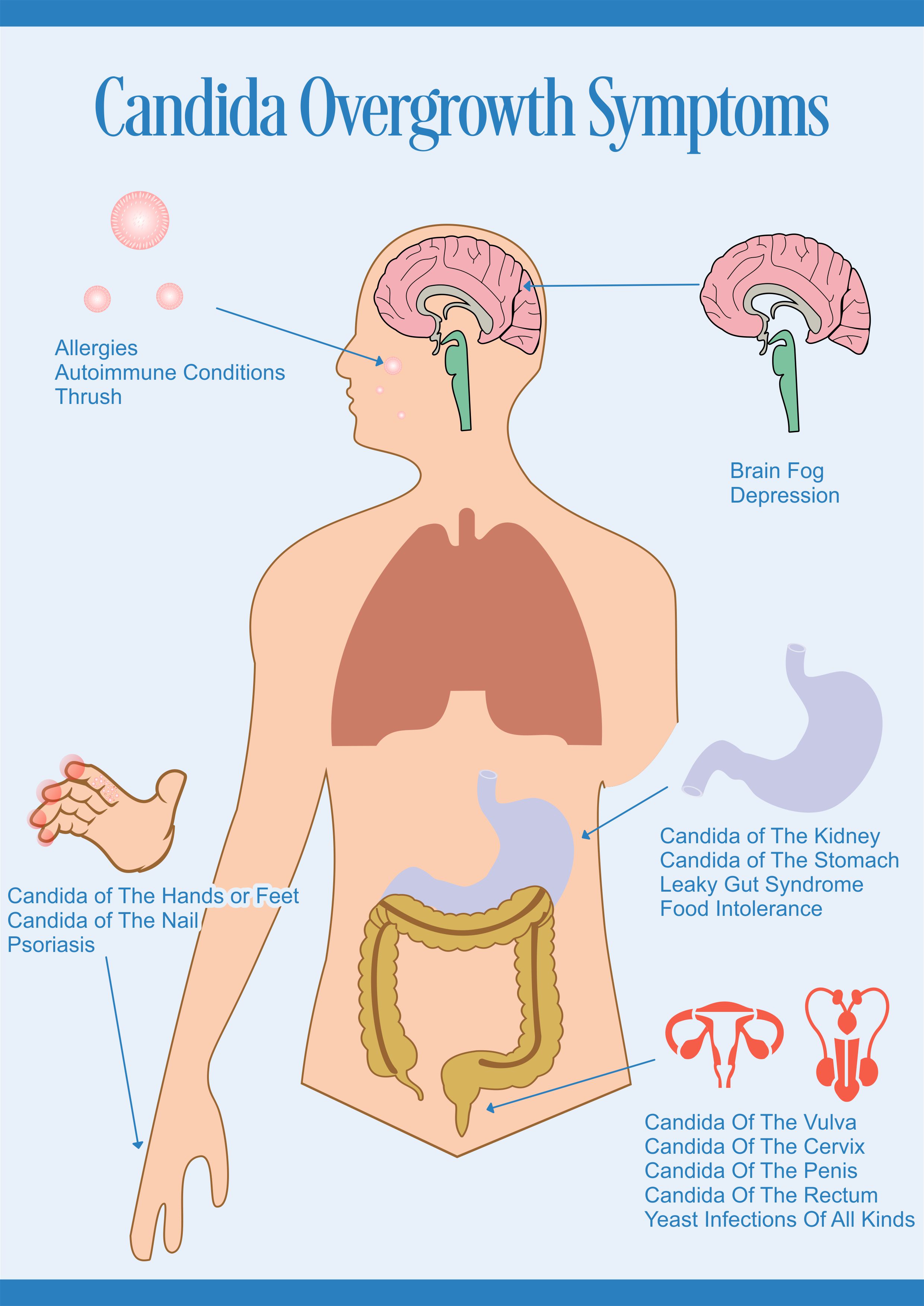
At this point, pathogenic bacteria and pathogenic mycelial Candida can end up taking root in the colon and are exceptionally hard to remove.
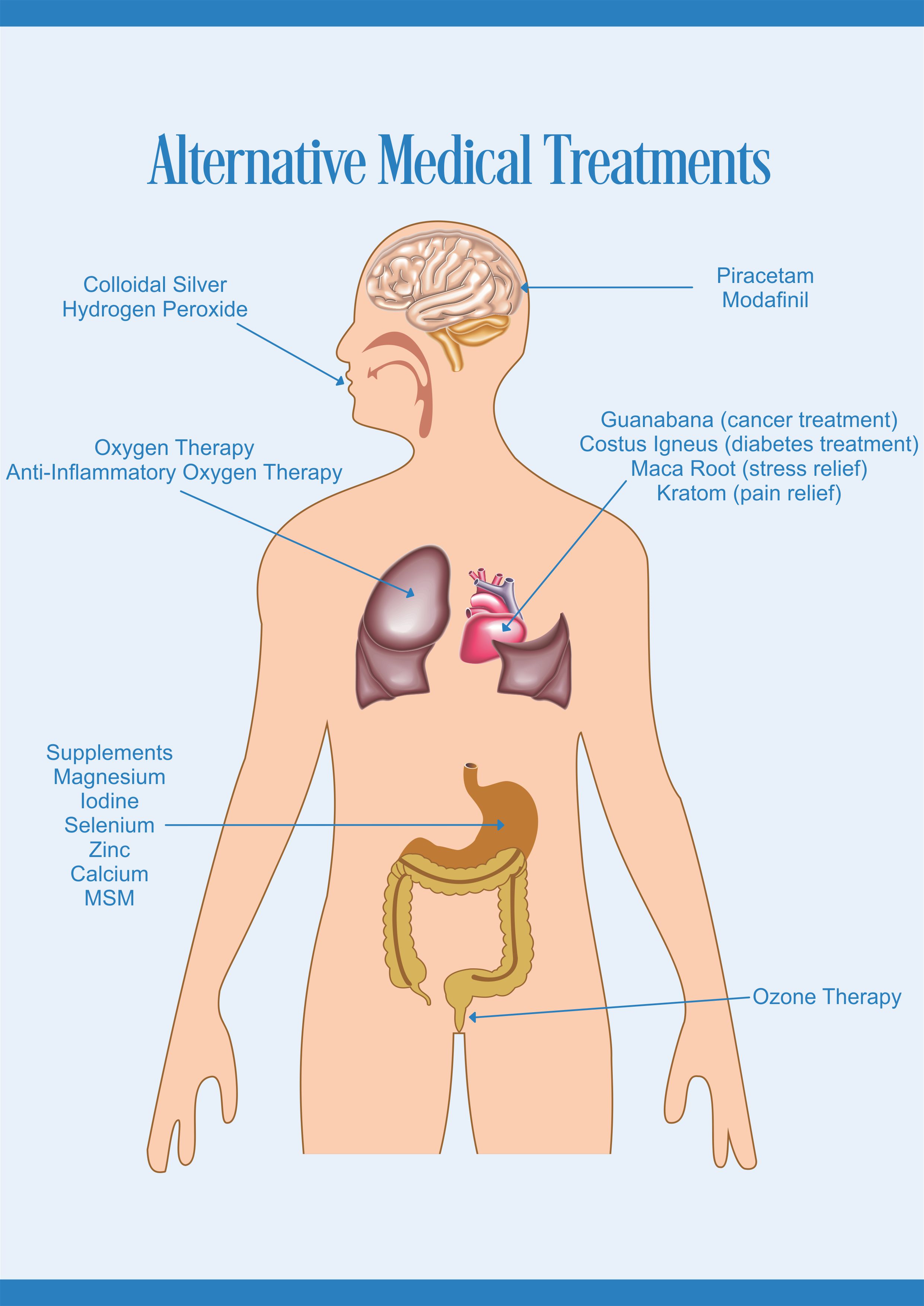
Iodine Can Replace Antibiotics
Instead of resorting to antibiotics, consider the benefit of iodine supplementation. Consuming internally or using iodine topically has the potential to treat bacterial infections without the unwanted side effects of antibiotics. Some of these side effects include death, compromised liver function, and a long-term bacterial / Candida imbalance.[xxii] In addition, the greater majority of the population is deficient in iodine, making supplementation an ideal preventative medicine.
Those who take part in a generic probiotic supplement regimen will likely not have much luck colonizing healthy bacteria at this point, as the breeding ground of the colon is already full of life forms that are not willing to give up their opportune positioning.
Realize that antibiotics still have their place in medical treatment, especially for life threatening bacterial infections. If antibiotic use is necessary, use with probiotics in order to reduce the overall side effects.
Another reason that probiotic supplementation on its own may be ineffective in this battle is because many times, pathogenic bacteria and fungi are protected by a thick layer of mucoid plaque that is difficult to penetrate. Those who have this type of problem need to focus on a colon cleanse program first and then attend to their bacterial imbalance.
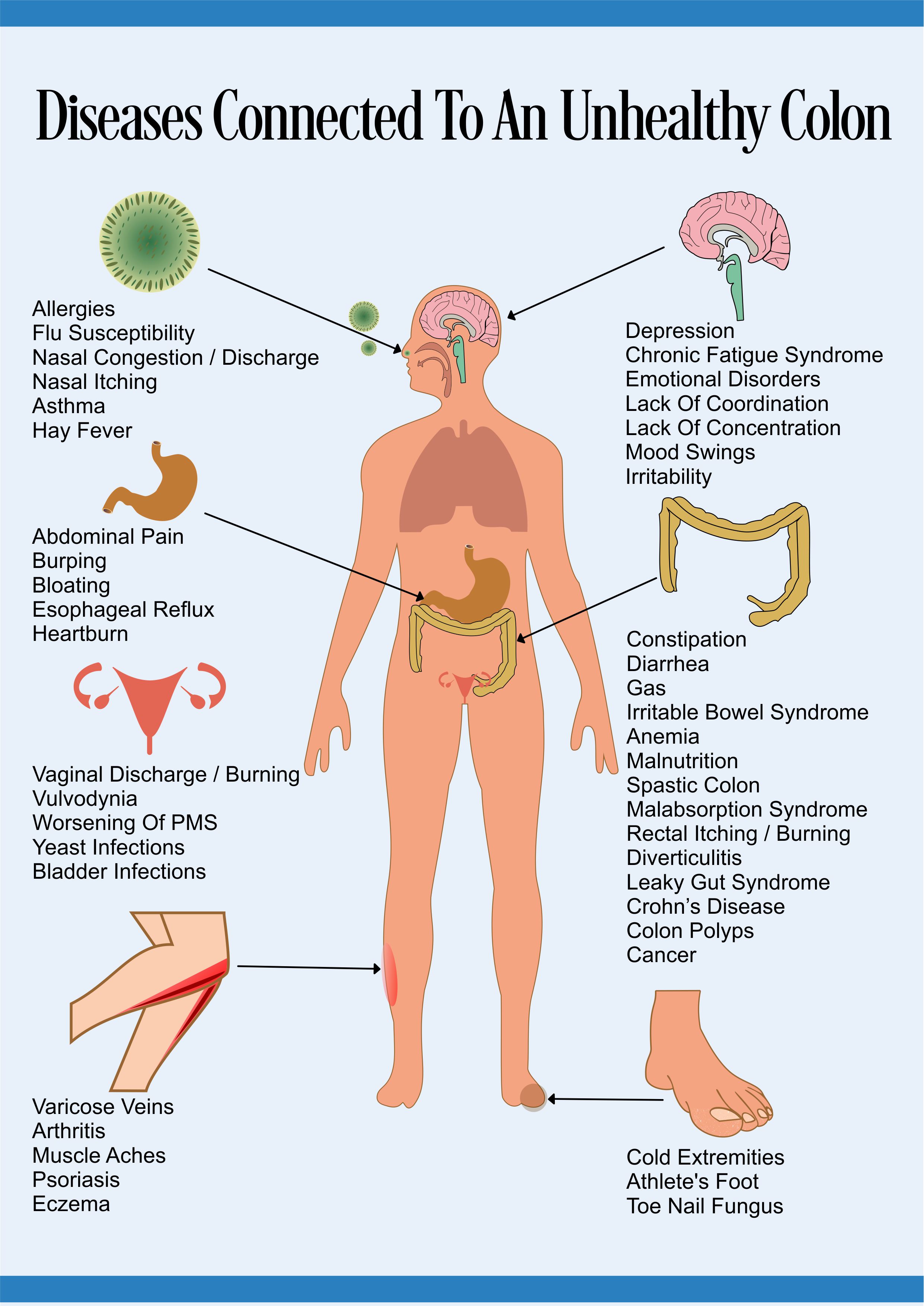
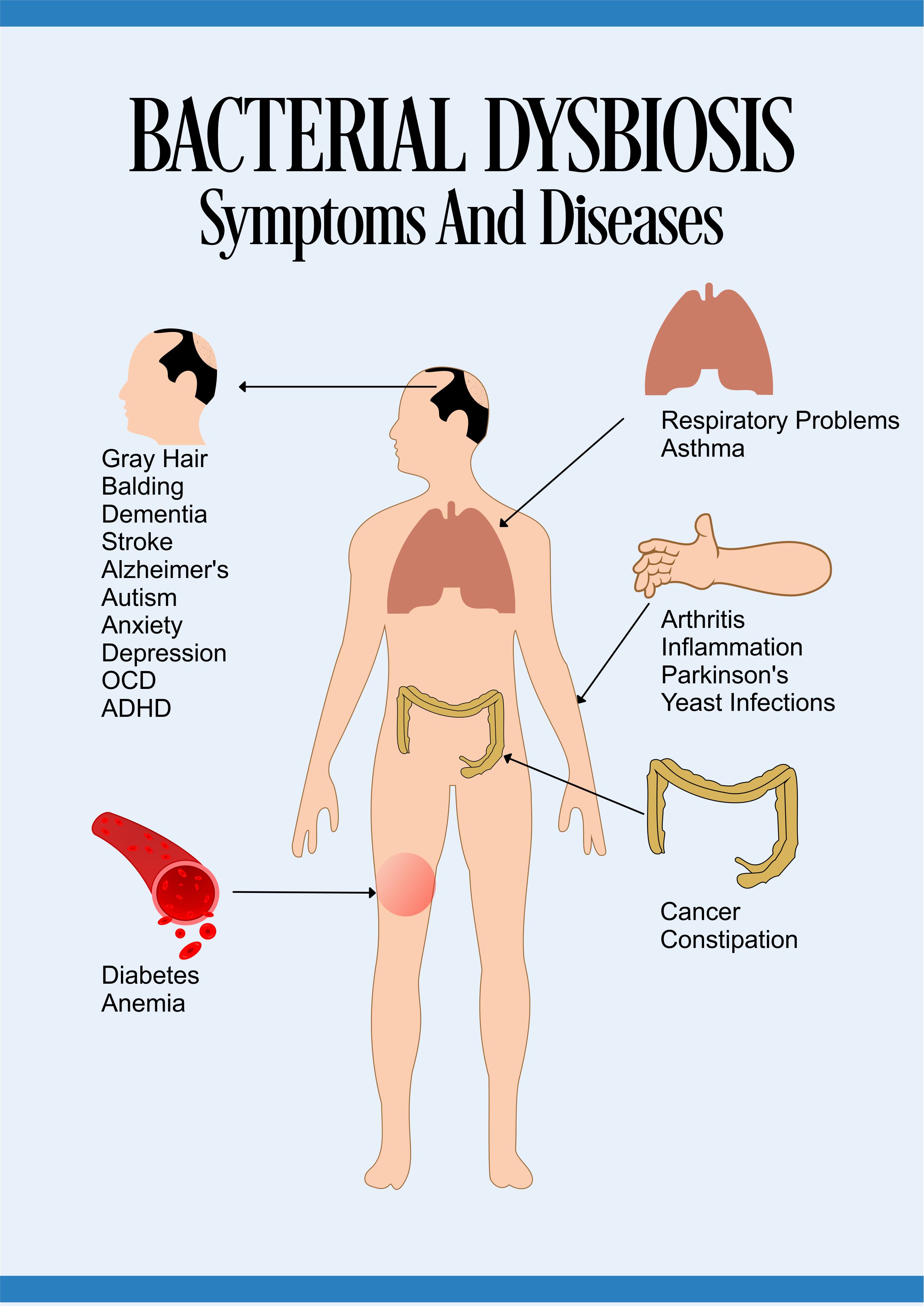
Symptoms And Diseases Associated With Bacterial Dysbiosis
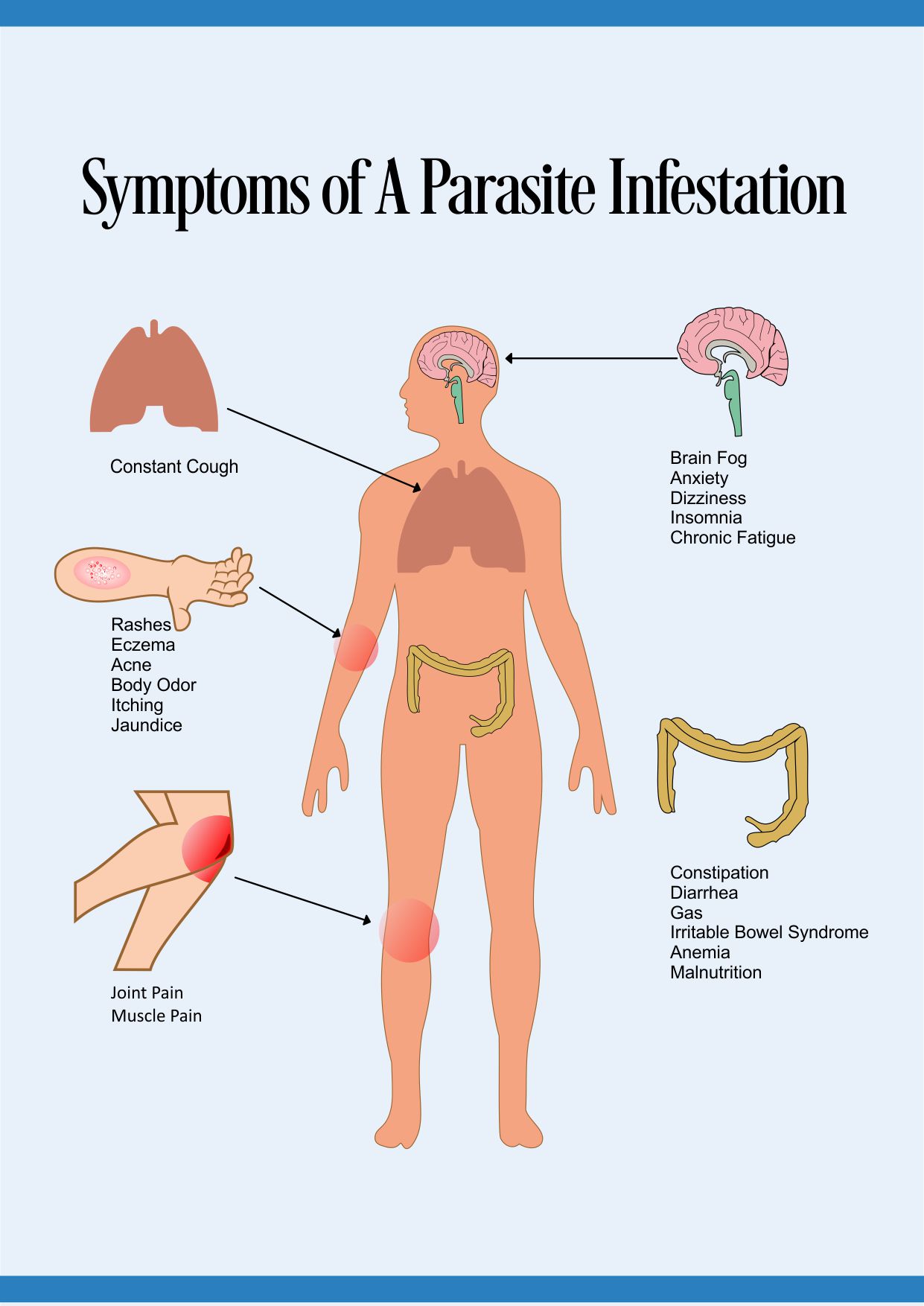
Those who don’t have a strong gut flora allow invasive pathogenic bacteria to colonize in their colon, including Shigella, Campylobacter, and Salmonella.[xxiii]
In addition, bacteria like Clostridium difficile can cause a whole host of potentially lethal problems for those who don’t have the proper intestinal flora.
Here are some of the symptoms and diseases associated with bacterial dysbiosis…
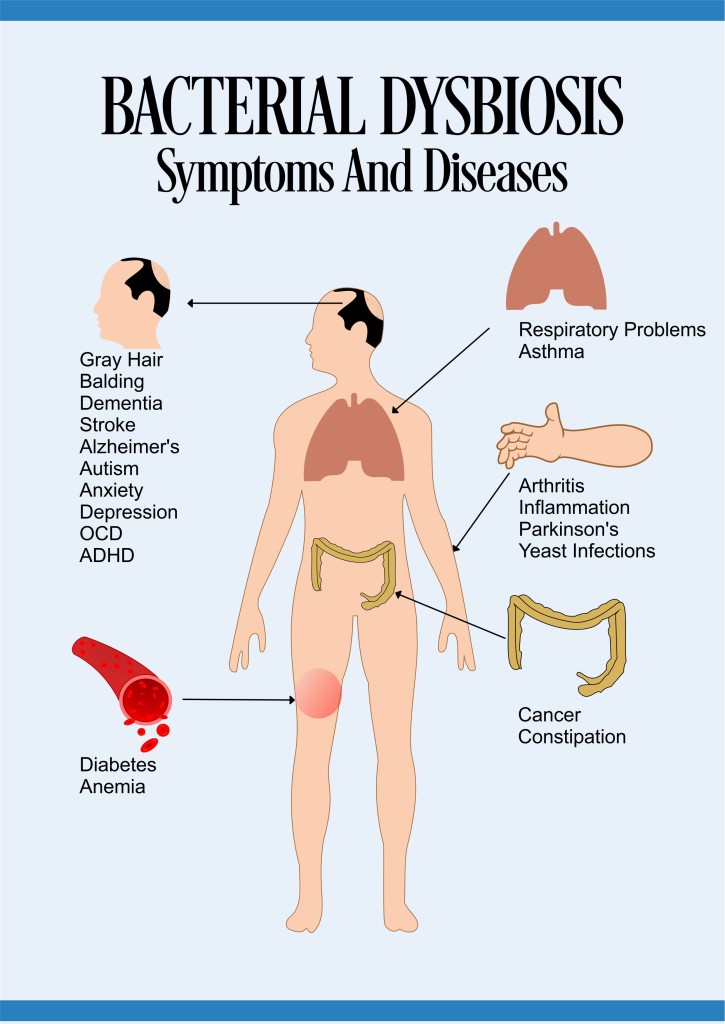
Share the Symptoms Of Bacterial Dysbiosis On Your Site
Gray hair, balding, dementia, diabetes, obesity, eczema, anemia, stroke, cancer, Parkinson’s, Alzheimer’s, constipation, arthritis, anxiety, depression, OCD, ADHD, autism, yeast infections, asthma, inflammation, autoimmune diseases, and respiratory problems, among others.[xxiv]
As more and more research is done on the association between the microbiome and diseases, the connection becomes even more obvious. Those who are suffering from any type of diseases should first balance their gut flora and see if that makes a difference before resorting to drastic procedures.
Individuals who suffer from bacterial dysbiosis often have a reduced rate of mucosal cell turnover, vascularity, baseline cytokine production, and a defective cell mediated immunity. In addition, those who don’t have the proper bacterial balance may have blood-clotting problems, while suffering from anemia and neurological problems. [xxv]
In the end, focus on creating a healthy gut flora by living a healthy lifestyle, avoid antibiotics, and take advantage of a high quality probiotic supplement.
The Gut Flora – Immune System Connection
The gut flora as a whole is the largest factor in immune system function. Good bacteria increase lymphocytes, increase interferons, increase cytokines, stimulate phagocytosis, and stimulate antibody formation.[xxvi]
The gut is known to house 70% of the functioning immune system[xxvii] and it is mediated through bacterial communication. Bacteria are the first line of defense in the innate immune system response, as it has the potential to send signals directly to the immune system.
Healthy bacteria initiate the gut associated lymphoid tissue (GALT) innate immune system response.[xxviii] This system allows the body to discriminate between healthy and pathogenic organisms.
This immuno regulator circuitry between GALT and microflora enables bacteria to chemically talk to the epithelium and provide innate immunity.[xxix]
Certain factors like Gc protein-derived Macrophage Activating Factor (GcMAF) assist the immune system by increasing macrophage activity.[xxx] While GcMAF remains at a healthy level in those with a balanced bacterial system, its presence is greatly reduced in those with chronic diseases, like cancer, AIDS, and colitis, which we will talk about later.
The take-home message is that a healthy microbiome is a necessity for all bodily systems to function optimally. Those who focus on maintaining a healthy intestinal flora will be able to allow their immune system to function properly, their neurological system to communicate adequately, and greatly reduce their susceptibility to chronic illnesses.
Removing Bad Bacteria From The Gut Flora
Pathogenic bacteria are generally living in the colon in response to some sort of stimulus. In individuals with a toxic buildup of fecal matter or undigested food throughout their intestines, pathogenic bacteria simply feed on this waste product.[xxxi] Those who remove this waste product will likely find that pathogenic bacteria leaves the system, as there is no more food for them to consume.
Probiotic Treatment
Probiotics
The best option currently available is to take a product like, Custom Probiotics, as they introduce billions of probiotic life forms into the digestive system.
The daily consumption of high-quality probiotics can reduce diarrhea, vaginitis, bloating, gas, lactose intolerance, indigestion, constipation, food allergies, and brain fog, among others.[xxxii]
In all reality, almost anyone can benefit from a high-quality probiotic supplement.
Using Food As Medicine
Fermented food like homemade kimchi, kefir milk, colostrum, Kombucha Tea and fermented raw milk are great ways to introduce probiotics into the digestive system.[xxxiii] Here is more information about eating right and living well.
A novel idea in order to promote healthy bacteria levels and immune system function is to ferment certain immune factors in a milk culture. There is a patented technique in order to create GcMAF through milk fermentation.[xxxiv] This could allow people to consume this immune factor and be able to fight off chronic diseases with one more weapon.
While there are currently GcMAF injections available, incorporating this into a food product is a tastier option. However, accessibility to GcMAF in the USA and UK appears to be limited due to regulations.[xxxv]
GcMAF has been shown to treat cancer and treat autism by Dr. Bradstreet and Dr. Gonzalez, both of whom mysteriously died this year. Those who want more information on these two doctors and their research findings should go here.
As a brief summary on their work, GcMAF effectively causes cancer cells to undergo apoptosis. It also neutralizes Nagalase, a component in vaccines and has been related to the development of Autism.
Prebiotics
Feed The Good Bacteria
As soon as symbiotic bacteria have been reintroduced into the colon, they need to be fed in order to properly flourish. These bacteria thrive on fiber; more specifically soluble fiber and those who wish to properly provide nutrition for symbiotic bacteria should eat well. Eating things like fruits, vegetables, properly prepared beans and even oat fiber allow bacteria to multiply. Those who want to include more fiber in their diets should consider eating more fruits, vegetables and beans or supplementing with oat fiber, if desired.
In addition, those who want to maintain their healthy bacteria should make intelligent lifestyle choices that affect their wellbeing. Live well and treat your body like a temple and it is likely to last for a long time.
Fecal Transplants
Clostridium difficile / Wikimedia Commons / Public Domain
Those who suffer from Clostridium difficile may consider taking advantage of a fecal transplant.[xxxvi] The success rate on removing this harmful pathogen from the bowels is quite high. Those who are interested in such a procedure should do further research.
Future Treatments
In the future, treating chronic diseases will likely focus on the microbiome, rather than the human element or the symptoms attributed to pathogens. Futuristic doctors will likely analyze a stool sample before anything else in order to obtain an accurate microbiome profile of a patient. Through this analysis, doctors will be able to diagnose disease and provide customized treatment options. These doctors can simply focus on improving the composition of the gut flora and revel as symptoms melt away.
Product Summary
Gut Flora Holds The Key To Good Health
An ideal probiotic program should accompany a pathogen removal program that includes removing mucoid plaque, pathogenic mycelial candida, and parasites. Those who follow the correct program when improving their gut flora have the potential to displace bad bacteria and Candida with symbiotic bacteria. At this point, living healthy and taking part in alternative medicine, when necessary can allow the body to remain in an ideal state.
Please share normalcolon.com with others who would benefit from this information.
[i] Mpkb.org,. ‘Microbes In The Human Body (MPKB)’. N.p., 2015. Web. 3 July 2015.
[ii] Nih.gov,. ‘NIH Human Microbiome Project Defines Normal Bacterial Makeup Of The Body’. N.p., 2015. Web. 10 July 2015.
[iii] Evans, J. M., L. S. Morris, and J. R. Marchesi. ‘The Gut Microbiome: The Role Of A Virtual Organ In The Endocrinology Of The Host’. Journal of Endocrinology 218.3 (2013): R37-R47. Web. 10 July 2015.
[iv] Funkhouser, Lisa J., and Seth R. Bordenstein. ‘Mom Knows Best: The Universality Of Maternal Microbial Transmission’. PLoS Biol 11.8 (2013): e1001631. Web. 10 July 2015.
[v] Gonzalez A, et al. ‘The Mind-Body-Microbial Continuum. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 26 July 2015.
[vi] YK, Hao. ‘Microflora Of The Gastrointestinal Tract: A Review. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 3 July 2015.
[vii] Brown, Kirsty et al. ‘Diet-Induced Dysbiosis Of The Intestinal Microbiota And The Effects On Immunity And Disease’. Nutrients 4.12 (2012): 1095-1119. Web. 10 July 2015.
[viii] Gorbach SL, et al. ‘Colonization Resistance Of The Human Intestinal Microflora: Testing The Hypothesis In Normal Volunteers. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 3 July 2015.
[ix] MJ, Hill. ‘Intestinal Flora And Endogenous Vitamin Synthesis. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 3 July 2015.
[x] NPR.org,. ‘Gut Bacteria Might Guide The Workings Of Our Minds’. N.p., 2013. Web. 3 July 2015.
[xi] Macfarlane, S., E. J. Woodmansey, and G. T. Macfarlane. ‘Colonization Of Mucin By Human Intestinal Bacteria And Establishment Of Biofilm Communities In A Two-Stage Continuous Culture System’. Applied and Environmental Microbiology 71.11 (2005): 7483-7492. Web. 10 July 2015.
[xii] Z, Stark. ‘In Vitro Production Of Short-Chain Fatty Acids By Bacterial Fermentation Of Dietary Fiber Compared With Effects Of Those Fibers On Hepatic Sterol S… – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 10 July 2015.
[xiii] Psychology Today,. ‘Your Backup Brain’. N.p., 2015. Web. 3 July 2015.
[xiv] http://www.apa.org,. ‘That Gut Feeling’. N.p., 2015. Web. 3 July 2015.
[xv] Aguilera M, et al. ‘Antibiotic-Induced Dysbiosis Alters Host-Bacterial Interactions And Leads To Colonic Sensory And Motor Changes In Mice. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 10 July 2015.
[xvi] GutSense.org,. ‘Gut Sense: How To Restore Intestinal Flora And Eliminate Constipation’. N.p., 2015. Web. 3 July 2015.
[xvii] Nrdc.org,. ‘Antibiotic Resistance | NRDC’. N.p., 2015. Web. 3 July 2015.
[xviii] GutSense.org,. ‘Gut Sense: How To Restore Intestinal Flora And Eliminate Constipation’. N.p., 2015. Web. 3 July 2015.
[xix] Peak-health-now.com,. ‘How Bile Protects You From Parasites And Candida’. N.p., 2015. Web. 10 July 2015.
[xx] Jonbarron.org,. ‘Stomach Acid’. N.p., 2007. Web. 3 July 2015.
[xxi] Croswell, A. et al. ‘Prolonged Impact Of Antibiotics On Intestinal Microbial Ecology And Susceptibility To Enteric Salmonella Infection’. Infection and Immunity 77.7 (2009): 2741-2753. Web. 10 July 2015.
[xxii] Dr. Sircus,. ‘Iodine And Antibiotics’. N.p., 2009. Web. 29 July 2015.
[xxiii] Atsu.edu,. ‘Infections Of The Large Intestine’. N.p., 2015. Web. 10 July 2015.
[xxiv] GutSense.org,. ‘Gut Sense: How To Restore Intestinal Flora And Eliminate Constipation’. N.p., 2015. Web. 3 July 2015.
[xxv] Canny, G. O., and B. A. McCormick. ‘Bacteria In The Intestine, Helpful Residents Or Enemies From Within?’. Infection and Immunity 76.8 (2008): 3360-3373. Web. 3 July 2015.
[xxvi] Wu, Hsin-Jung, and Eric Wu. ‘The Role Of Gut Microbiota In Immune Homeostasis And Autoimmunity’. Gut Microbes 3.1 (2012): 4-14. Web. 3 July 2015.
[xxvii] Vighi, G. et al. ‘Allergy And The Gastrointestinal System’. Clinical & Experimental Immunology 153 (2008): 3-6. Web. 3 July 2015.
[xxviii] Rhee KJ, et al. ‘Role Of Commensal Bacteria In Development Of Gut-Associated Lymphoid Tissues And Preimmune Antibody Repertoire. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 10 July 2015.
[xxix] WA, Forchielli. ‘The Role Of Gut-Associated Lymphoid Tissues And Mucosal Defence. – Pubmed – NCBI’. Ncbi.nlm.nih.gov. N.p., 2015. Web. 10 July 2015.
[xxx] Faim.org,. ‘Gcmaf For The Treatment Of Cancer, Autism, Inflammation, Viral And Bacterial Disease | Foundation For Alternative And Integrative Medicine’. N.p., 2015. Web. 4 July 2015.
[xxxi] Medicalinsider.com,. ‘Mucoid Plaque’. N.p., 2015. Web. 10 July 2015.
[xxxii] Probiotics.org,. ‘Lactobacillus Acidophilus Benefits & Side Effects — Probiotics.Org’. N.p., 2015. Web. 4 July 2015.
[xxxiii] Mama, Katie. ‘Health Benefits Of Fermented Foods – Wellness Mama’. Wellness Mama. N.p., 2011. Web. 10 July 2015.
[xxxiv] Gcmaf.se,. ‘Bravo Probiotic’. N.p., 2015. Web. 10 July 2015.
[xxxv] Gov.uk,. ‘Regulator Warns Against Gcmaf Made In Unlicensed Facility In Cambridgeshire – Press Releases – GOV.UK’. N.p., 2015. Web. 10 July 2015.
[xxxvi] Brandt, Lawrence. ‘Fecal Transplantation For The Treatment Of Clostridium Difficile Infection’. Gastroenterology & Hepatology 8.3 (2012): 191. Web. 4 July 2015.